Special Education
Special Education
Special Education is specially designed instruction, support and services provided to students with an identified disability requiring an individually designed instructional program to meet their unique learning needs. Special education and related services are available to eligible students of ages 2 through 25 at Vikas learning centre to students with ASD and paediatric neuro cases.
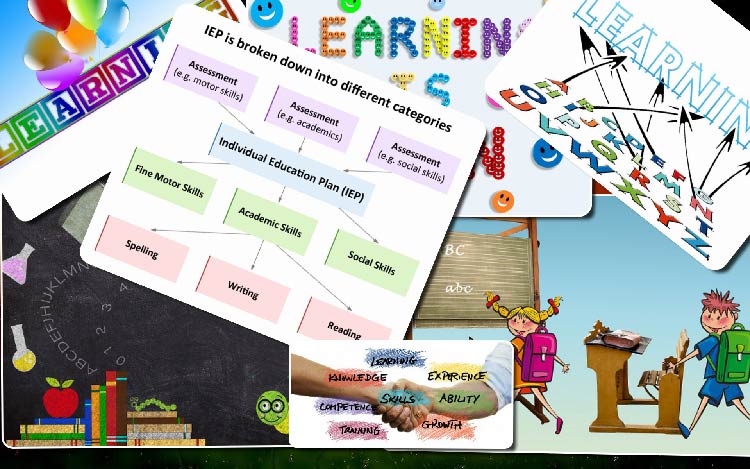
The IEP provides a description and action plan of what the child with disability requires in terms of services and supports necessary to learn. It is a prerequisite to receiving special education services.
Special educator just as the general education teacher offers knowledge and expertise relative to the general education curriculum. The special education teacher has more in depth background on how to teach learners with special needs. They use that knowledge and experience to offer ideas for modifying the curriculum, individualizing instruction, suggesting behavior management techniques, and presenting progress data. In many cases, the special education teacher is also the child case manager, he or she is responsible for organizing meetings and tracking goal progress throughout the school year.
What is special education?
What do you imagine when you think about special education? You might picture children with disabilities spending the day tucked away in a different kind of classroom, separated from most of the kids their age. This may have been the norm in the past. But as the field of special education has moved forward, much has changed.
Special education today is still focused on helping children with disabilities learn. But this no longer has to mean placing kids in a special classroom all day long. In fact, federal law requires that students who receive special education services be taught alongside their non-disabled peers as much as possible.
For example, some students with dyslexia may spend most of the day in a general education classroom. They may spend just an hour or two in a resource room working with a specialist on reading and other skills. Other students with dyslexia might need more support than that. And others might need to attend a different school that specializes in teaching kids with learning disabilities.
“Special education refers to a range of services that can be provided in different ways and in different settings.”
There is no “one size fits all” approach to special education. It’s tailored to meet each student’s needs. Special education refers to a range of services that can be provided in different ways and in different settings.
If your child qualifies for special education, he’ll receive individualized teaching and other key resources at no cost to you. The child will focus on his strengths as well as his challenges. And you’ll be an important member of the team that decides what he needs to make progress in school.
What disabilities are covered by special education?
IDEA covers 13 types of disabilities. These categories include autism, hearing impairment and intellectual disability (which used to be referred to as “mental retardation”). Another category, called “specific learning disability,” applies to many kids who have learning and attention issues.
A specific learning disability most often affects skills in reading, writing, listening, speaking, reasoning and doing math. Common learning issues in this category include:
- Dyslexia: Difficulty with reading, writing, spelling, speaking
- Dyscalculia: Difficulty doing math problems, understanding time and money, remembering math facts
- Dysgraphia: Difficulty with handwriting, spelling, organizing ideas
- Dyspraxia: Difficulty with hand-eye coordination, balance, fine motor skills
- Auditory processing disorder: Difficulty interpreting what the ear hears (which is different from having a hearing impairment)
- Visual processing issues: Difficulty interpreting what the eye sees (which is different from having a visual impairment)
There’s a separate category called “other health impairment.” It’s defined as having limited strength or alertness, which affects educational performance. Children with attention-deficit hyperactivity disorder (ADHD) are often covered by this category.
IEP must describe, discuss, and ultimately make recommendations with respect to;
Current performance, which is frequently called “present level of performance”
-
- Annual goal and objectives
- Assessment
- Services
- Transition
- The behaviour intervention plan and functional behaviour Assessment, as needed
- Placement
The IEP is written collaboratively with the faculty and parents of Vikas learning centre. The plan is executed and continuous assessments are done and modifications to the plan as deemed necessary are done to meet the needs of the child.
Speech Therapy
Speech Therapy
Individual Support Plan (ISP) describes, discusses, and ultimately make recommendations with respect to;
- Current performance, which is frequently called “present level of performance”
- Goal and objectives
- Assessment
- Services
Early Intervention Therapy
Early Intervention Therapy
Sensory Integration Therapy
Sensory Integration Therapy
Sensory Integration Therapy for Sensory
processing disorders and Dyslexia.
Sensory integration therapy is designed to help kids with sensory processing issues. This type of therapy aims to adjust the way children respond to physical sensations. It is based on the idea that some kids experience ‘sensory over load’ and are oversensitive to certain types of stimulation. When children have sensory overload, their brain have trouble processing or filtering many sensation at once. Meanwhile, other kids are under sensitive to some kinds of stimulation. Kids who are under sensitive don’t process sensory messages quickly or efficiently.
These children may seem disconnected from their environment. Sensory integration therapy exposes children to sensory stimulation in a structured, repetitive manner. The theory behind this treatment approach is that, over time, the brain will adapt and allow them to process and react to sensation more efficiently.
Sensory integration is a subconscious and automatic neurological process that occurs in every person at all stages of life. Our brains take in information thorough our senses and organize. It so that we are able to respond appropriately to particular situations and environmental demands. Sensory experiences include touch, movement, body position, vision, smell, taste, sound and the pull of gravity.
Sensory integration therapy uses repetitive exercise to help a child experience other sensations more accurately. An intervention study involves observing the child in the class room and while at play. Parents are interviewed and an assessment is done. Based on that, recommendations are made which best suits the child and a plan of action is charted.
Autism’s symptoms often include difficulty processing sensory information such as textures, sounds, smells, tastes, brightness and movement. These difficulties can make ordinary situations feel overwhelming. As such, they can interfere with daily function and even isolate individuals and their families.
Sensory integration therapy, as practiced by occupational therapists, uses play activities in ways designed to change how the brain reacts to touch, sound, sight and movement. While the therapy is not new, it has remained somewhat controversial. “Part of the problem has been the many different techniques that have been used under the name sensory integration.
“The rationale is that by changing how sensations are processed by the brain, we help children with autism make better sense of the information they receive and use it to better participate in everyday tasks
For most people sensory integration develops in the course of ordinary childhood activities. When a person has good sensory integration then they are able to process information automatically and efficiently. But for some people, sensory integration does not develop as efficiently as it should and can affect activities of daily living, academic achievement, behavior or social participation.
Children can present with different types of sensory integration difficulties (also known as sensory processing processing difficulties).
These include:
Hyper (over) sensitive
- Fear of heights
- Dislike of touch experiences eg nail cutting, messy play, hair cutting
- Dislike of loud and sudden sounds
- Avoidance of playground equipment (swing and slides)
Hypo (under) sensitive
- appears to have no fear or doesn’t feel pain
- Seeks movement or touch opportunities’ (fidgets, rocks, run about, leans on peers)
- mouth or chew things
- poor attention to the environment or people around
Motor Planning (praxis)
- Appears clumsy
- Difficulty creating movements ideas
- Difficulty planning and executing new movements
Poor posture
- Slouches at desk
- Fidgets/difficulty sitting in one position for extend period of time
- Impact on fine motor coordination & ball skills
- Impact on fine motor coordination & ball skills
- Poor Balance
Sensory integration provides occupational therapists with a frame work for assessing and treating children who present with difficulties outlined above.
Different ways an occupational therapist may use an sensory integration approach:
- Direct 1:1 therapy using specialized equipment
- Provision of a sensory diet and sensory based therapeutic activities for home and school (see “calming and altering activities activity ideas” information sheet-coming soon)
- Environmental adaptations at home and school (see ‘coping with classroom environment strategies’ information sheet – coming soon).
- Consultation & education with careers and school.
Some areas of involvement are:
- Balance and posture
- Muscle tone and strength
- Environmental adaptations at home and school (see ‘coping with classroom environment strategies’ information sheet – coming soon).
- Body awareness
- Fine motor abilities (pinching and grasping, manipulative skills, pencil and scissors use, hand writing)
- Gross motor abilities (running, jumping, climbing)
- Motor planning (ability to plan, initiate and execute a motor act)
- Visual perception (shape recognition, visual memory)
- Visual motor integration (copying shapes, copying block design)
- Sensory integration (response to sensory stimuli, discrimination of sensory input)
- Behaviour Modification (arousal level, attention, problem solving skills)
- Self-care skills (eating , toilet habits, bathing)
- Community living skills (management of money, shopping)
- Pre academic skills (identify letters, sounds, shapes, colours and numbers)
- Play skills are used as a tool to enhance life skills.
- Social skills.
Standardized Assessments are conducted on a regular basis. These Assessments are for motor proficiency, visual perception, hand writing skills and sensory processing. These skills are evaluated and progress reports are sent to the parents along with their academic reports. Parents are trained at school so that they can continue the therapy at home to maintain continuity and regularity.
Some areas of involvement are:
Sensory process (or sensory integration) is the way in which the central nervous system of the body receives messages from the senses of the body and uses that information to act in appropriate motor or behavioral responses. Sensory processing disorder (SPD, also known as sensory integration dysfunction) is a condition in which the sensory signals received by the central nervous system do not become organized into an appropriate response. A child who has SPD may find it challenging to process and act appropriately his or her central nervous system receives sensory information which causes problems with carrying out activities of daily living. SPD can cause tremendous challenges for a child if it is not treated or managed appropriately.
Sensory processing disorder may affect only one sense – such as sight or hearing – or it can impact multiple senses and impacts each child in a different way. One child may react strongly to different textures of clothing while another may over-respond to loud sounds. Children with SPD may also have impairments of the joints and muscles, impacting posture and motor skills. Many children who have SPD are not immediately diagnosed with the condition as the disorder can be mistaken for ADHD. While this disorder is commonly diagnosed in childhood, many people reach adulthood without a proper diagnosis and may struggle with the symptoms of the disorder.
Children who have sensory processing disorder are effectively treated by a combination of physical and occupational therapy that focuses upon activities that strengthen a child’s ability to handle sensory stimuli appropriately. Over time, a child will learn to appropriately respond to sensory stimuli so that they are able to behave in a more positive manner in therapy, in school, and at home.
How does one determine which sensory perception areas should be trained?
If the child displays more than one deficiency in the following areas, then these areas of sensory perception should be trained:
Visual recognition
- Basic essentials cannot be understood from what is seen
- Visually similar things are not recognized as different
- Distinguishing important information from a multitude of stimuli is unsuccessful
- The ability to filter something out of the background is lacking
- The child must touch/handle everything in order to understand it
- Difficulties with distinguishing between colours and shapes
- Writing and recognition of letters is difficult
- Handwriting is untidy and difficult to read
- Lack of uniformity in the size of the letters
- Uneven reproduction of letters and numbers
- Confusion between letters which are different in placement (d/b, u/n)
- The ability to distinguish between visually similar letters, arithmetical symbols, and numbers (h-k, a-o, 7-4, 6-5) is severely lacking
- Inverted (left to right or right to left) reading or writing of numbers, for example 6 and 9
- Increasingly occurring copy errors
- Difficulties grasping amounts
- Omission of letters or numbers
- Difficulties with quantities over ten
- Difficulties with compound arithmetic problems
- Difficulties with structuring text exercises
Visual memory
- Visual information is not retrained
- Difficulties in recognizing colours, shapes, images, patterns, and objects
- Memorization of word images does not succeed: words are often written properly ten times, then incorrectly again
- Difficulties with drawing patterns from memory
- Transposition of letters a-e-o, h-k, f-t, m-n
- The child cannot find his place in the text when reading
- Frequently checking the pattern while copying
- The writing is angular, curvatures and lengths are different
- The letters a-e-o appear the same
Visual sequencing
- Visual sequences cannot be perceived properly
- Difficulties with grasping the succession of letters when reading together
- Reversing the sequence of letters when reading and writing
- Letters or syllables are missing, they are transposed or added
- Halting, slow reading
- Assistance articulating, prompting of a given text
- Switching the word order when writing
- Omission of letters, endings or words when writing
- Duplication of letters
- Frequent subsequent additions of missing letters in a word
- Uneven line spacing and spaces of the letters within a word as well as between the words
- Reversal of the sequence of a story (for instance, while writing compositions)
- Distraction by small details and losing the place in the story
- Incorrect sequencing of numbers, omission of digits
- Difficulties counting and counting off
- Difficulties grasping amounts
- Slow learning of basic arithmetic skills
- Omission of intermediate steps when doing arithmetic
Acoustical recognition
- The basics of the sounds heard cannot be grasped
- The ability to distinguish whether sounds are the same or not is severely lacking
- A sound is matched with the wrong letter
- Removing a letter from a word does not work
- Inability to distinguish between or transposition of similarly sounding noises, words or numbers
- Ability to distinguish between vocalized and non-vocalized consonants is severely lacking: g-k, b-p, d-t, s-z, f-v
- Ability to distinguish between diphthongs is severely lacking: ei-eu, eu-au
- Transposition of elongation and sharpening
- Difficulties distinguishing between m and n, for example between 3. and 4. case
- Difficulties repeating the same or similar words
- Difficulties repeating unfamiliar words
- Difficulties transcribing a series of spoken words
Acoustical memory
- Cannot remember and repeat what was heard
- Frequent questions when reciting
- Omissions or additions of letters, syllables or words
- Failure to complete recitations
- Severe difficulty understanding what was heard
- Errors with b/p, d/t, g/k
- Poor vocabulary, frequent repetitions of words
- Short compositions with poor content
- Prompting of sentences
- Omission of parts of verbally assigned arithmetic problems
- Assistance articulating, prompting of a given text or arithmetic problem
Acoustical sequencing
- Acoustical sequences are not perceived correctly
- Muddled explanations, loses the thread easily
- Difficulties with verbally presenting sentences with the correct word order and placed correctly in the thought process
- Difficulties avoiding becoming distracted by minor details when telling a story
- Halting, broken speech with inharmonious breathing
Spatial orientation
- Spatial perception is not judged correctly
- Ability to judge spatial and temporal measures (distances, amounts, and units) is severely lacking
- Difficulties orienting oneself in an unfamiliar environment
- Memorizing a specified route is tiring
- Building to a pattern or blueprint (building games) is unsuccessful
- Difficulties learning to tell time
- Very slow learning to dress oneself
- Riding a bicycle and swimming are learned much later
- Ability to imitate rhythmic movements is severely lacking
- Problems with singing and movement games
- Ignoring given spatial instructions
- Uneven line spacing
- Cannot arrange the lines properly, writing outside the margins
- Losing the line when reading
- Inverted writing (right to left instead of left to right)
- Transposition of letters when distinguishing their position: b-d, b-p
- Numbers are transposed: 6-9, 36-63
Body perception
- Difficulties orienting oneself to one’s own body
- Confusion between right-left, above-below, behind-before (in back of-in front of)
Occupational Therapy
Occupational Therapy
Occupational Therapy enables students to improve their development and prevents disability from impacting their functioning in daily life. It also focuses on the promotion, restoration and mainstreaming of productivity in people with wide range of abilities and disabilities.
Occupational Therapy may include adaptations of task or environment to achieve maximum independence to enhance the quality of life. Occupational therapy has a definite role in helping / treating children with sensory processing deficits.
Occupational Therapists aim at enabling the child to be as physically, psychologically and socially independent as possible. Occupational therapists work with children who have inadequate motor coordination and planning (praxis), sensory processing dysfunction, social-emotional imbalance, impaired cognitive functions, poor academic performance and limited play skills.
Occupational Therapists use a knowledge base of neurology, anatomy, physiology, kinesiology, child development and child psychology, psycho social development, activity analysis, and therapeutic techniques. They are trained to treat clients holistically, addressing their cognitive, emotional, and physical needs through functional, activity-based treatment. When working in paediatrics, occupational therapists select activities that are of interest and have meaning for children, and that also meet therapeutic goals.
What is Occupational Therapy?
Many people think the word “Occupation” is a work related term: however, an occupation can be anything someone does to occupy his or her time in everyday life. Groups of activities constitute an occupatio9n. For Example, work, leisure / play and self-care are general occupation. Within each of these are components of one or more activities. Self-care includes many activities of daily living such as brushing your teeth, bathing, eating, and dressing. Leisure / play. Can involve reading, writing, teaching, or typing. Activities are the building blocks or components of human occupation.
“Occupational therapy is an allied health profession concerned with improving a person’s occupational performance. In a pediatric setting, the occupational therapist deals with children whose occupations are usually play, preschoolers, or students.





























The ISP is written collaboratively, with the parents and faculty of Vikas learning centre. Continuous monitoring of the ISP is done and required actions are done to help the child with special needs.